Adobe StockSave this storySave this story
Adobe StockSave this storySave this story
I’ve never had a pimple in my life. I’m bragging, I know.
But it’s an important detail, along with the fact that I’ve been a beauty journalist for nearly seven years—which means I know my skin, and I know when something is off. So when a spot arrived in the very center of my forehead in August 2023, I figured it was about time I got my first zit.
Only, this “zit” didn’t go away. It scabbed over, scarred, and expanded from a tiny dot to a quarter-sized discolored blotch on my forehead where a unicorn horn would be over the course of a few months. Then, around six weeks later, came a second spot. I ran through every possible explanation: a reaction to skin care, a chemical burn from a pimple patch, maybe even a curse from a past life. My most Googled phrase that year was “ingredients for fading scars,” and no amount of niacinamide or tranexamic, kojic, or azelaic acid made a difference.
The writer in December 2023, about four months since the “zit” initially appeared.
Courtesy of subject
Eventually, I booked a dermatologist appointment. The doctor thought it could be psoriasis; I was sticking with my chemical burn theory. A biopsy came back: seborrheic dermatitis. Spoiler alert—it wasn’t. Turns out, the procedure didn’t paint the entire picture because it was a shave biopsy and didn’t get to the full root of the issue, just scraping the surface. So when I applied the prescribed steroid faithfully, nothing changed. The lesions had signed a lease in perpetuity and neither triamcinolone acetonide nor betamethasone dipropionate could evict them.
With my self-esteem unraveling, I booked another appointment—this time at a different practice. Claudia Slutzky, a certified physician assistant at True Dermatology in New York City, took one look and told me that it wasn’t dermatitis. The clues? “This patch was so well demarcated right in the center of [your] forehead, and nothing seemed to help,” she’d told me.
When two more spots appeared on my chest two months later, following the same bump–scab–scar pattern, Slutzky raised the possibility I least expected: lupus. Dr. House always said it’s never lupus, so how could it be lupus? No one in my family had it, and in my head lupus was a “disease,” not something that could show up on my face. Shocked, I asked her: “Do you know what it means to say the word ‘lupus’ to a Black woman?” She did, and she was just as upset as I was. Black women are disproportionately affected by lupus, according to the Centers for Disease Control and Prevention (CDC). In fact, says the organization, Black, American Indian, and Alaskan Native women are two to three times more likely than white women to develop lupus, and tend to have more severe cases when they do. The CDC also states that on average, Black people with lupus die at younger ages—by more than a decade—than white people with lupus. All that in mind, the word “lupus” carries a deep cultural trauma for a lot of Black women, and I was—and am—one of them.
After consulting with her supervising physician, Amy Spizuoco, a board-certified dermatologist at the same practice, they performed a punch biopsy, which goes deeper than the surface-level one I’d had a year prior. When the results came back around a week later, we had an answer: discoid lupus erythematosus, a chronic autoimmune condition that causes rashes on the skin and face. What I thought was a simple blemish was actually a diagnosis that would change my life—and my identity.
What is Discoid Lupus Erythematosus?
Discoid lupus erythematosus (DLE) is a chronic autoimmune condition that affects the skin, often in sun-exposed areas like the face, scalp, and ears. It can look very different depending on your skin tone. “In darker skin tones discoid lupus may appear as pink, gray, or purple lesions,” says Patricia Oyetakin, MD, a board-certified dermatologist based in Atlanta. “In lighter skin tones it is more pink or red.” Over time, lesions may lead to scarring, pigment changes, or even hair loss, though these features usually emerge later—one reason early diagnosis is so challenging.
Some key red flags: pigment changes that don’t resolve, scarring or thickening of the skin following a lesion, hair loss on the scalp as a result of lesions, and lesions clustered in areas like the face, scalp, and ears that are often exposed to the sun. Early discoid lupus (DLE) can mimic acne because both may appear as red or inflamed bumps. The key differences are persistence and after-effects. “Unlike acne, DLE lesions often develop scaling, follicular plugging, and occur in sun-exposed areas,” says dermatologist Pooja Rambhia, MD, a board-certified dermatologist based in New York City. “They don’t resolve within a typical acne cycle and instead can linger for weeks to months. DLE lesions are also more likely to leave behind scarring or pigment changes, while acne usually heals without such pronounced, long-lasting marks.”
Lupus comes in many forms. Selena Gomez, for example, has lupus nephritis, which is an inflammation of the kidneys caused by systemic lupus erythematosus (SLE). SLE is also an autoimmune disease, but it can affect the entire body, including the heart, lungs, kidneys, and joints. The main difference between my form of lupus and other variations of the disease is that discoid lupus is cutaneous, or limited to the skin. “Only five percent of individuals with discoid lupus will go on to develop SLE,” explains Meggan Mackay, MD, a board-certified rheumatologist based in New York City. “But individuals with discoid lupus should be aware of symptoms such as joint pain, hair loss, and overwhelming fatigue, as this could indicate SLE.”
DLE is the most common form of chronic cutaneous lupus, but it’s still relatively rare. It most often affects women between the ages of 20 and 50, and people with skin of color face both a higher risk and more severe side effects from the disease, including scarring alopecia, a form of permanent hair loss caused by inflammation that destroys hair follicles. In DLE, scalp lesions can damage the follicle beyond repair, leading to irreversible bald patches that cannot regrow hair even after the disease is controlled.
Why Discoid Lupus Is Often Misdiagnosed
I was fully prepared to accept my first dermatologist’s diagnosis of seborrheic dermatitis. They’re the experts, right? My story isn’t unusual, especially as a Black woman. We’ve all heard the myths: “Black people don’t need sunscreen” or “melanoma is less likely to develop in darker skin.” Those ideas fuel a pattern where our skin concerns are often minimized.
Plus, conditions can present differently on different skin tones, and there has historically been less education that focuses on dark skin for dermatologists. The American Academy of Dermatology (AAD) has put vast efforts into diversifying their training materials and unlearning medical bias, most recently working in collaboration with the Skin of Color Society to assure that images used in dermatologic education demonstrated how conditions present in all skin tones, called the Clinical Image Collection. “By incorporating a diversity of images into professional dermatology education material, we can empower dermatologists and other clinicians to improve their diagnostic skills and enhance patient care for all,” a representative for AAD told me. “The ultimate goal is for the AAD Clinical Image Collection to become the largest, most-trusted and comprehensive source for skin disease images.”
In skin of color, discoid lupus can be especially deceptive. DLE often presents with pigment changes that look like post-inflammatory hyperpigmentation. On deeper skin tones, redness—a classic sign in lighter skin—is far less visible. “DLE can be misidentified, especially early on, because the lesions can mimic common conditions like acne, eczema, or seborrheic dermatitis,” Dr. Rambhia explains. “Even with biopsy, subtle findings or sampling error can sometimes delay the correct diagnosis."
“Black patients experience more frequent and severe disease damage, including prominent ear and scalp dyspigmentation and scarring alopecia, as compared to non-Black patients,” she continues. “The visual impact of pigmentary changes is often more significant in patients with darker skin tones, emphasizing the importance of early recognition and treatment to prevent permanent scarring and disfigurement.”
How DLE Affects More Than Skin
The hardest part wasn’t just the lesions—it was watching my face change in slow motion, feeling myself disappear. I was truly handling an ego death on top of a chronic illness. To you, this may be vanity; for me, it was my entire identity. It got so bad that the scars—which, by April 2024, had multiplied to two spots smack-dab in the middle of my forehead—were the only thing I could see when I looked in the mirror. I would cry when I saw myself without makeup—my self-esteem, which I had considered to be unshakeable after a lifetime of building it up, was destroyed. Not just because of the spots on my face, but because I felt so vain for even allowing my self-worth to be harmed so easily. I felt like the only thing anyone could see were the spots.
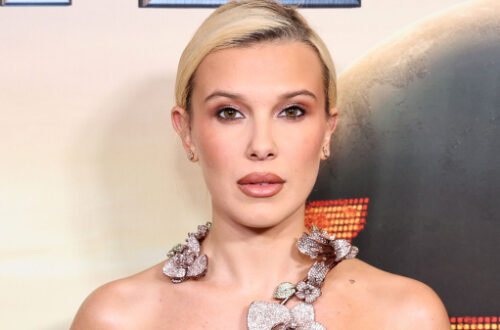
The writer seen here in March 2024, by which time she says the scars had darkened.
Courtesy of subject
Psychologist Sari Chait, PhD, was not surprised to hear about these emotions. “When someone develops visible changes over time, like scarring or lesions, it can be difficult to incorporate your new visual appearance into the picture you already have of yourself. That discrepancy alone can cause distress and can lead to one feeling significant loss,” she says. “In many ways, that sense of loss of what one used to look like is a form of grief.” I have been known to have a “boy who cried wolf” view of the world, feeling that my cries for help have always been diminished by my overdramatic nature. But I had to advocate for myself—I couldn’t let two spots on my forehead get in the way of my life.
And as a Black woman, the pressure was doubled. My hair could be undone—I’d just throw on a wig and keep moving. But my skin? That was supposed to be untouchable. “Image is very important in Black communities; [there’s an unspoken rule of] ‘don’t look like what you’re going through,’” says therapist Vatara Scott, a licensed clinical social worker in North Carolina. “When that image is not on par with our own or others’ expectations, it can feel shaming or disparaging. Rather than it being a reflection of a chronic condition… it can easily be regarded as a lack of care or upkeep.”
That stigma only deepened my spiral. DLE wasn’t just changing my skin—it was rewriting how I saw myself.
How to Treat DLE
Once I had a name for what was happening to my skin, the next big question was: What now? Discoid lupus erythematosus doesn’t have a cure, but it can be managed—and the earlier treatment begins, the better the chance of preventing scarring and pigment changes. Dr. Rambhia explains that managing DLE usually focuses on reducing inflammation, preventing flare-ups, and minimizing permanent damage like scarring.
“Medical treatment includes a combination of topical anti-inflammatory medications and oral treatments,” explains Dr. Oyetakin. “I explain to my patients that topical steroids can be safely used as a ‘fire extinguisher’ to quickly calm down intense itching and burning. Topical non-steroid medications can then be used as long-term maintenance. In severe cases, oral immunosuppressant medications are effective and should be closely managed.” When I first received my lupus diagnosis, Slutzky and Dr. Spizuoco prescribed me a stronger triamcinolone cream, just to see if a higher dose of steroids might do the trick. When it didn't, they moved me to a regimen of Opzelura cream—a JAK inhibitor (a newer class of oral or topical medications that block key inflammatory pathways in the immune system) used to treat mild to moderate eczema and nonsegmental vitiligo—along with ammonium lactate lotion to treat the dry scaly skin, and Tazorac—the brand name for the prescription topical retinoid tazarotene—to assist with the inflammation.
Lifestyle strategies are just as important: “Stress is our number one nemesis in our day-to-day lives,” Dr. Oyetakin adds. “It not only affects mental health, it also causes flare-ups in inflammatory skin conditions. I discuss stress management strategies with my patients as an important part of our management plan.” With all forms of lupus, sun protection is crucial. Dr. Oyetakin says that broad-spectrum sunscreen, sun-protective clothing, and even oral antioxidant supplements like polypodium leucotomos, a tropical fern native to Central and South America which has been shown to have benefits in photosensitive conditions like lupus, are all essential tools. If sunscreen was a passion for me before, now it’s a matter of survival.
For many patients, systemic medications like the ones I’m on are necessary. “The current treatments of choice include oral hydroxychloroquine, topical corticosteroids, other strong anti-inflammatory medications, and local corticosteroid injections,” says Dr. Mackay. But new options are on the horizon: “Research into the molecular mechanisms for discoid lupus and SLE has resulted in the development of new drugs called biologic therapies that target specific pathways causing disease and may be more effective than the traditional treatments.”
Victoria Werth, MD, a board-certified dermatologist and medical advisor to the Lupus Research Alliance, is also hopeful. “Several phase one, two, and three trials are studying drugs that seem to work more quickly and more often than current treatments. While CLE is more common and more severe in people with skin of color, we know these populations are less likely to join trials. It is essential to increase participation to correctly assess if the therapies are working for everyone.”
How to Advocate for Yourself
I cannot overstate how much I recognize that getting to the point of a diagnosis is a privilege. Lack of access to proper medical care is an issue across the board, and I am lucky enough to know that I work in a field that not only puts me in front of some of dermatology’s best minds, but also allows me to (somewhat) afford the expensive creams and medications I need to keep my DLE at bay. There is not a single complaint in my world when it comes to that, and staying grateful and hopeful is the only thing that kept me going through the last few years.
By the time I finally got my diagnosis, I realized the only reason I made it there was because I kept pushing. That meant trusting my gut when prescriptions didn’t work, when the biopsy didn’t explain what I saw in the mirror, and when my mental health was unraveling. This problem literally lived on my face—I couldn’t ignore it.
“If your condition is not responding to the current treatment plan, always talk to your provider,” says Slutzky. “There can be multiple ways to treat a condition, and every patient can respond differently.”
Dr. Spizuoco notes that even dermatologists face tough calls: “The gold standard of diagnosis of autoimmune conditions of the skin is a biopsy. Many times these lesions are on the face, and it’s very difficult… because we know a biopsy will leave a scar. And that’s what we are trying to avoid.” I’m convinced that’s why my first biopsy missed the mark. For purely cosmetic purposes, we didn’t want to punch a hole in the middle of my forehead during the initial biopsy and risk an even worse scar developing in its place. Unfortunately, that meant the shave didn’t go deep enough to get to the actual root of the issue. In the end, trusting my instincts—and saying yes to a deeper biopsy for the lesions on my chest—changed everything.
Self-advocacy also means being prepared for how my lupus might change in the future. “It is extremely helpful for patients to keep track of the appearance of the rash—if it has improved, stayed the same, or worsened—and whether any new lesions have developed,” says Dr. Mackay. “If you have other concerns like new joint pain or hair loss, be prepared to discuss these. Even if the provider does not have an answer, at least the symptom will be considered and addressed.”
And beyond the exam room, advocacy can be collective. “If we are to improve therapies for CLE we will need to facilitate and complete these trials,” says Dr. Werth. Patients showing up in research data ensures that future treatments actually work for the people most affected.
For me, advocating meant refusing to accept “just dermatitis” as the final word. For you, it might mean asking for a second opinion, keeping a symptom diary, or finding a support group. Whatever the path, it starts with believing yourself when your body—or your skin—tells you something’s wrong.
When I first walked into True Dermatology in January, I was genuinely afraid that I was, well, a monster. Working with Slutzky did more than that. When I told her I was writing this story, I said I wanted it to be about us—because we did this together. Throughout the experience, she often told me that the emotional side of this diagnosis is just as important as the objective medical side. Our nine months of appointments weren’t just about creams or biopsies; they were about building trust. That comfort she gave me is what allowed us to get to the best place I’ve been so far. Dr Spizuoco, who guided us through the hard calls, reminded me that chronic conditions like this take teamwork. “Chronic skin conditions require a partnership between the patient and the dermatologist,” she explained. And that’s exactly what I had: a team that was willing to listen when I said, “This isn’t getting better,” and to believe me when I cried in their office because it felt like I was losing my face.
Now, my spots are slowly and gradually fading thanks to topical meds, and I’m working with a rheumatologist on the oral treatments I need to keep my DLE in check. What I thought was a bump on my face turned out to be a hurdle in my life, but it’s one I’m learning to live with. I’m being gentler with myself, reminding myself that my skin doesn’t define my worth—and yes, I am obsessively wearing sunscreen.
Because in the end, this isn’t just about a diagnosis. My mother wanted me to love my Black skin more than anything else, and I do. It’s also about what can happen when you refuse to stop asking questions, when your providers trust you enough to dig deeper, and when you let yourself believe that your skin—even scarred, even imperfect—is still worth loving.